Hypothermia in children and infants occurs when core body temperature drops below the normal range of 36.5°C, usually due to the environment being significantly colder than the infant’s body temperature (e.g., cold, damp). Unlike adults, infants and babies cannot effectively regulate their body temperature due to their smaller size and limited fat stores.
With their larger surface area relative to their body weight, they can lose heat rapidly, particularly when exposed to cold surroundings.
Mild cold stress can have far-reaching consequences on a baby’s respiration, circulation, and overall wellness. In newborns and premature infants, even mild-to-moderate cases of hypothermia may cause low blood sugar or poor feeding. Severe cases could lead to extremely serious complications that could be life-threatening.
The following information discusses everything you need to know regarding hypothermia in infants, including the causes, signs and symptoms, potential treatments, and preventative measures that may be employed. Regardless of whether you are a new parent, care provider, or childcare professional, learning to identify the first signs of hypothermia in your infant will help keep them safe and healthy.
What Is Hypothermia?
Hypothermia occurs when a baby’s core body temperature drops below 36.5°C, preventing the body from functioning normally. At this lowered temperature, vital processes such as metabolism, breathing, and circulation begin to slow. A baby’s heart rate may decrease, breathing can become shallow, and the body may struggle to maintain energy levels needed for growth and survival.
A baby’s small size, limited fat reserves, and immature ability to regulate body temperature make them more prone to heat loss than older children and adults. Infants are susceptible to temperature changes, even from brief exposure to cold or wet conditions.
Early intervention is important in order to reduce the risk of negative health outcomes and avoid more serious complications. Quick responses to these conditions will allow your infant to achieve a full recovery as soon as possible.
What Causes Hypothermia in Babies and Children
Several everyday factors can make an infant or child lose body heat quickly. Understanding these causes is the first step in preventing hypothermia.
- Cold environment or draught: Many houses are very cold. A baby or child can lose a lot of body heat very quickly if in a room below the recommended temperature for that age group. Even being in a room for a short time (10-30 minutes) can be dangerous for a newborn, infant, or toddler.
- Wet skin or clothing: When a child is wet after bathing, swimming, or being outside in the rain, if they do not dry immediately, they will lose a lot of body heat quickly through evaporation. Wet clothes and bedding make the situation worse because they continue to draw heat from the body.
- Premature and low-weight babies: Babies born too soon (premature) or with a low birth weight have less body fat and are not able to regulate their temperature as well as full-term, normal-weight babies. These babies are at higher risk of developing cold stress.
- Illness or infections: Certain illnesses and infections (fever, sepsis, low energy, and dehydration) can weaken an infant or child’s ability to generate body heat. They are at a greater risk of developing hypothermia when they are ill.
- Inadequate clothing or wrapping: Wearing clothing that is too thin or not covering the head and feet, or using blankets, can lead to significant loss of body heat even in otherwise warm environments.
- Outdoor exposure in cold weather (children): Older children can develop hypothermia if they spend an extended period outside in cold air due to wind or in wet conditions without proper clothing.
Being aware of these common causes is crucial, as early recognition and simple preventive measures can protect both babies and children from hypothermia.
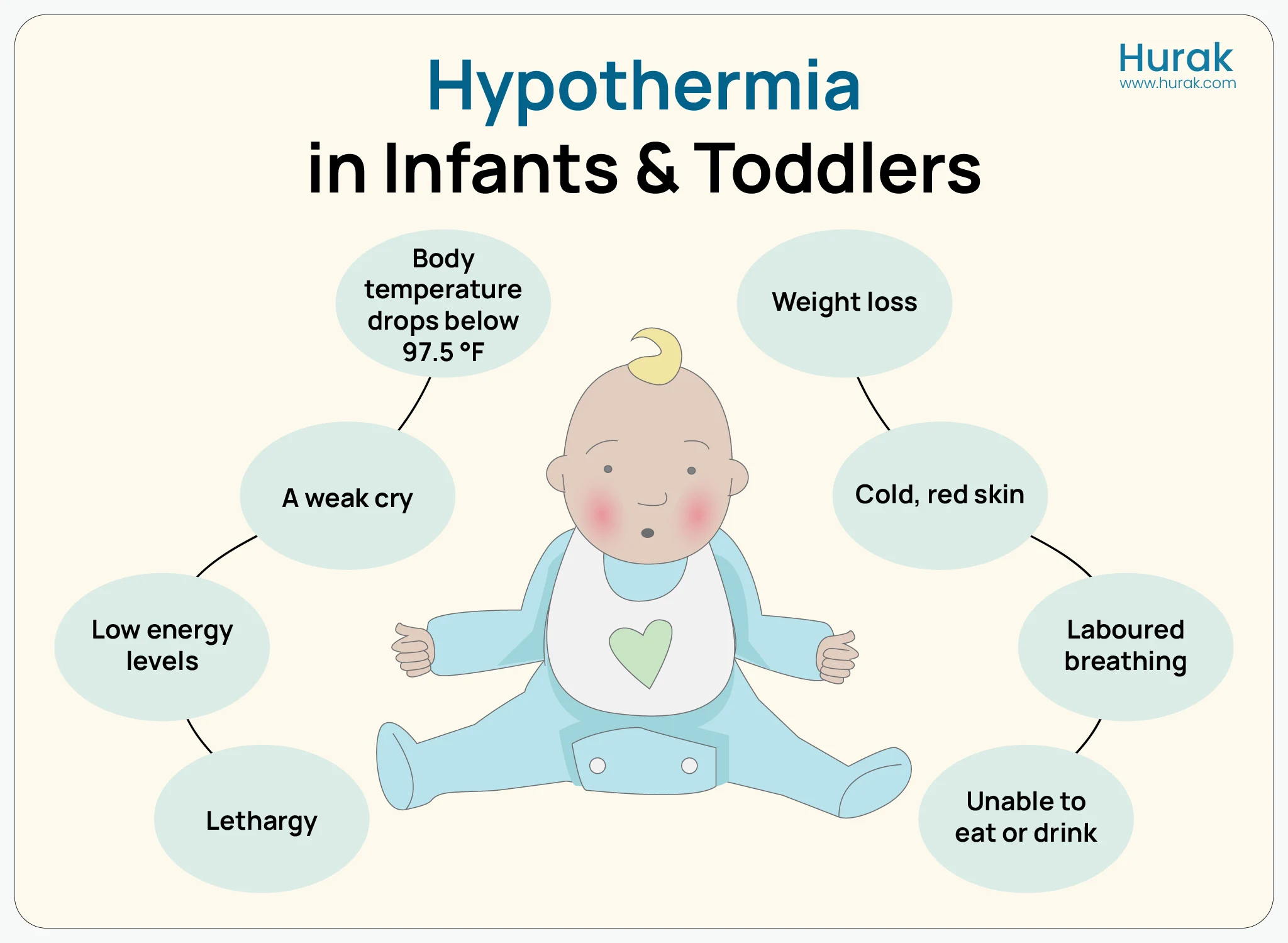
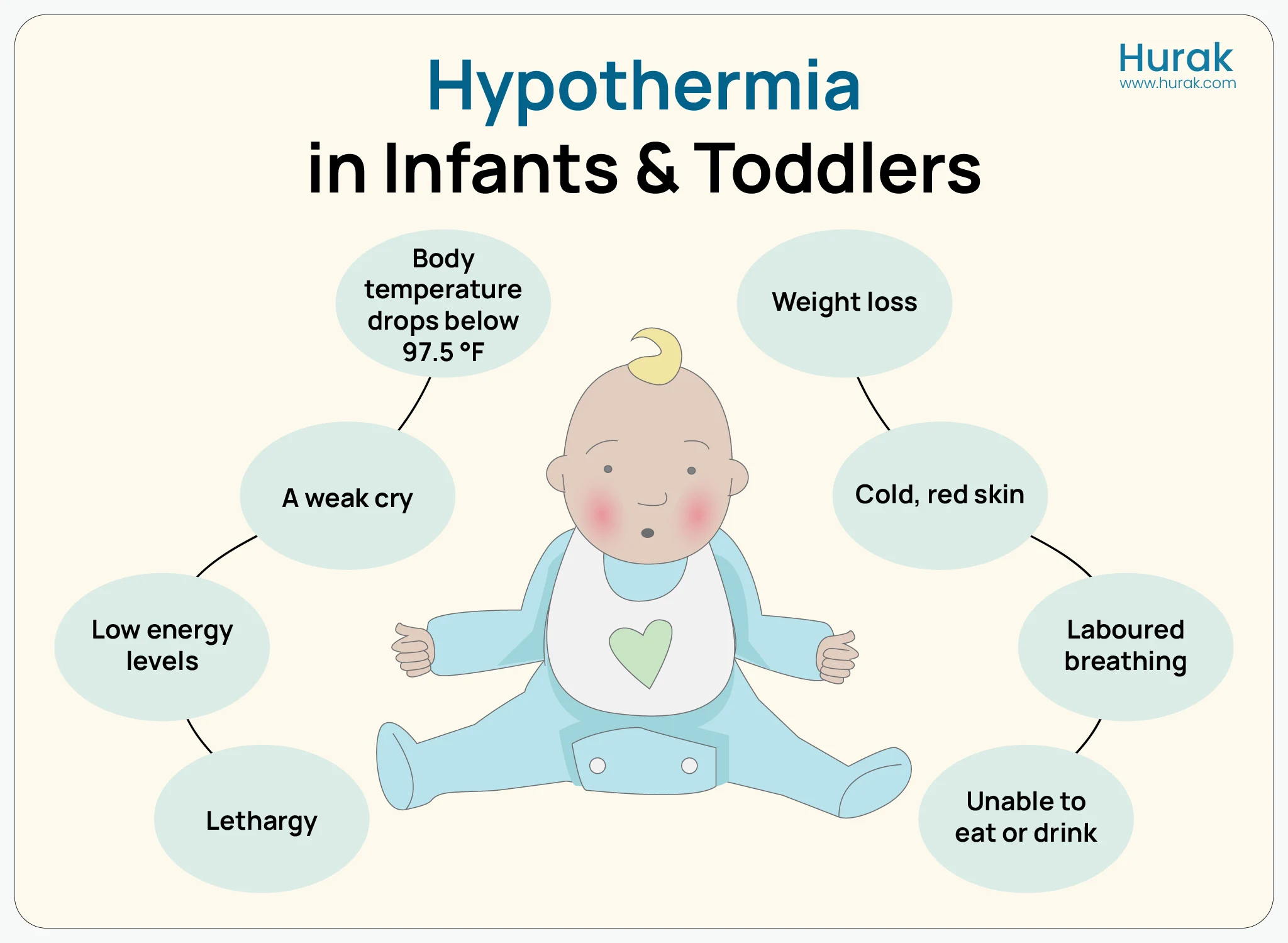
Signs and Symptoms of Hypothermia in Babies
Young children and babies cannot always tell us when they feel cold, so it is essential for carers and parents to recognise the warning signs early. Observing both physical cues and behavioural changes can help identify hypothermia before it becomes serious.
| Age Group |
Physical Signs |
Behavioural Symptoms |
| Babies / Infants |
Cold, pale, or bluish skin (hands, feet, lips); mottled skin; shivering (sometimes absent); cool abdomen or chest when touched |
Weak or high-pitched cry; slow or shallow breathing; poor feeding or refusal to feed; drowsiness, lethargy, reduced movement |
| Children / Toddlers |
Cold or pale skin; blue lips or fingers; shivering; numb extremities; slow capillary refill |
Shivering, tiredness or fatigue; irritability; complaints of feeling cold; clumsiness or poor coordination |
Important:
- A baby with a temperature below 36.5°C should always be treated as at risk.
- For older children, persistent cold skin, blue lips, unrelenting shivering, or unusual tiredness or confusion are warning signs.
When to call a doctor:
- Babies / Infants: Blue lips or face, very slow or shallow breathing, refusal to feed, unresponsiveness.
- Children / Toddlers: Persistent shivering, lethargy, confusion, cold extremities, or complaints of severe chill.
Prompt action and early recognition can prevent serious complications and ensure both babies and children stay safe and healthy.
How to Treat Hypothermia in Babies and Children
When a baby or child shows signs of hypothermia, it is essential to warm them gently and gradually. Sudden or aggressive warming can be harmful, so a calm and measured approach is necessary.
Mild Hypothermia – Babies / Infants
- Move the baby to a warm, quiet space away from draughts.
- Remove any wet clothing and dry the baby gently with soft towels.
- Wrap the baby snugly in warm blankets to retain body heat.
- Encourage skin-to-skin contact with a carer (kangaroo care) to help transfer warmth naturally.
- If the baby is alert, encourage feeding to maintain energy levels.
Mild Hypothermia – Children / Toddlers
- Move the child to a warm, draft-free room.
- Remove wet clothing and dry thoroughly.
- Wrap the child in warm blankets and offer warm drinks if the child is alert.
- Encourage gentle movement to generate body heat.
Moderate or Severe Hypothermia – Babies and Children
- Seek medical help immediately, as professional care is required.
- In hospitals, doctors may use incubators, radiant warmers, or warm intravenous fluids to safely restore body temperature.
- Warming must be gradual, as rapid increases in body temperature can cause shock or other complications.
- Monitor breathing, responsiveness, and temperature closely.
With prompt and careful treatment, most babies recover quickly and safely. Early recognition and timely intervention make all the difference in preventing serious complications. For caregivers interested in understanding the skills and techniques involved, this complete guide to first aid training levels provides detailed information about child care.
Possible Health Risks and Complications
If hypothermia in babies goes untreated, several health issues can arise. A baby with a temperature below 36.5°C should be treated as at risk.
- Breathing difficulties or irregular heartbeat: Low body temperature can slow respiration and affect heart function, placing additional strain on the baby’s body.
- Low blood sugar and metabolic imbalance: Hypothermia increases the risk of hypoglycaemia and disrupts normal metabolic processes, potentially affecting energy levels and growth.
- Weakened immune system and higher infection risk: Cold stress can reduce the body’s ability to fight infections, making babies more susceptible to illness.
While these complications are severe, early recognition and prompt treatment are highly effective. With proper care, most babies recover fully and safely.
Preventing Hypothermia: Tips for Babies and Children
The most important thing that parents or caregivers can do to help protect a child from cold stress is to take preventive measures. The preventative steps below will help you keep your baby safe and healthy.
- Keep the room warm at about 25–28°C
- Dry the baby right away after bathing (to prevent heat loss).
- Dress in layers (soft clothing with a hat and socks) to help keep in body heat.
- Practice skin-to-skin contact; holding your baby close against your chest is a natural way to help keep him/her warm.
- Avoid drafts (keep your baby away from windows, fans or air vents, which may cause a drop in body temperature).
- Check your baby’s temperature regularly (especially when it is cold outside or your baby is sick).
Early recognition and simple preventive measures can protect both babies and children from hypothermia.
Conclusion
Baby hypothermia can develop quickly, often due to cold environments, wet clothing, prematurity, illness, or inadequate wrapping. Recognising the early warning signs, such as freezing or bluish skin, weak cry, poor feeding, and lethargy, is essential for timely intervention. Mild cases can be managed at home with gentle warming and skin-to-skin contact, while moderate or severe hypothermia requires immediate medical attention.
Prevention is straightforward: maintain a warm environment, dress babies appropriately, dry them promptly, practise skin-to-skin contact, and monitor their temperature regularly. Knowledge and quick response can make a vital difference in keeping infants safe and healthy.
With proper awareness and care, cold stress in newborns can be prevented, ensuring your little one stays warm, healthy, and safe. Knowing the benefits of first aid techniques can help parents respond quickly and safely if their baby shows signs of hypothermia.
Frequently Asked Questions
What is hypothermia in babies?
It’s when a baby’s body temperature drops below 36.5°C, affecting breathing, metabolism, and circulation.
What causes hypothermia in babies?
Cold rooms, wet clothing, prematurity, illness, or inadequate wrapping can all cause heat loss.
What are the signs of hypothermia in babies?
Cold or bluish skin, weak cry, poor feeding, slow breathing, and lethargy.
How do you treat hypothermia in babies?
Mild cases: warm room, dry clothing, blankets, skin-to-skin contact. Severe cases: seek medical help immediately.
How can hypothermia in babies be prevented?
Keep rooms warm, dress in layers, dry promptly, practise skin-to-skin contact, and monitor temperature.
When should I call a doctor?
If the baby shows persistent cold, blue lips, a weak cry, slow breathing, refusal to feed, or lethargy.
Broaden Your First Aid Knowledge
Stay prepared and confident by exploring our additional first aid courses. Each one is designed to help you protect lives and promote safety wherever you are:
- Emergency First Aid at Work (1 Day): Learn core techniques like CPR and handling unconscious casualties, a perfect first step for beginners.
- First Aid at Work (3 Days): Gain full workplace certification while mastering complex scenarios such as burns, fractures, and cardiac emergencies.
- Paediatric First Aid (2 Days): Tailored for child-focused environments, this course equips you to respond effectively to choking, allergic reactions, and injuries in children.
- Basic First Aid Course: A valuable but straightforward introduction for families, volunteers, and community workers.
- Advanced First Aid Training: Develop advanced decision-making skills for serious emergencies involving multiple injuries or trauma.
- First Aid for Mental Health: Learn to approach, listen, and support those experiencing mental health challenges.