A baby choking is every parent’s worst nightmare. It happens suddenly, while playing, feeding, or even when the baby is lying down. Babies naturally put objects in their mouths as they explore and learn about the world. Choking accidents are more common than many people think.
Understanding what to do if your baby is choking can make a life-saving difference. Whether it’s a piece of food, a small object or milk going the wrong way, knowing the proper first aid steps and how to position your baby correctly can help clear their airway quickly and safely.
In this step-by-step guide, you will learn everything parents and caregivers need to know about baby choking first aid, from spotting the signs of choking to what to do when a newborn chokes on milk and how to stop a baby choking safely and confidently.
Understanding Baby Choking
Choking occurs when something blocks a baby’s airway, making it difficult or impossible for them to breathe. It can happen suddenly during feeding, while playing or even when the baby is lying down. Babies explore the world with their mouths, which makes them especially vulnerable.
Difference Between Gagging and Choking
It’s essential to understand the difference between gagging and choking. Gagging is the baby’s natural reflex to clear the throat. The baby may cough or make noises and can usually breathe. Choking, however, is a more serious issue. The airway is either wholly or partially blocked, and the baby may be unable to cry, cough, or breathe.
Why babies are more prone to choking
Babies are naturally at a higher risk of choking because their bodies and reflexes are still developing. Understanding the reasons can help parents take simple precautions to keep their little ones safe during feeding and playtime.
- Small airways: A baby’s airway is very narrow, so even a tiny piece of food, a toy, or an object can block it. This makes them more vulnerable to choking compared to older children or adults.
- Exploring with their mouths: Babies learn about the world by putting things in their mouths. It’s part of how they explore. Unfortunately, this curiosity often leads to them mouthing objects that are unsafe or too small to chew.
- Newborn feeding: During feeding, especially in newborns, milk can sometimes flow into the airway instead of the stomach. This can happen due to improper feeding positions or fast-flow nipples.
Due to their small airways and natural curiosity, babies require constant supervision when eating or playing. Being alert and prepared can significantly reduce the risk of choking.
Signs of Baby Choking
Recognising choking in a baby as soon as it happens can make all the difference in how effectively you respond. Babies can’t always signal distress clearly, so parents and carers need to know what to look for to recognise it. Understanding the warning signs early helps you act fast and potentially save a life.
- Inability to make sounds or cry
If your baby suddenly stops making any noise while feeding or playing, it may indicate that their airway is completely blocked. If the baby cannot cry, cough, or make any sound, this is a clear indication that air is not passing adequately, and you need to act quickly.
- Weak or no cough
Coughing is the body’s natural defence mechanism for clearing the airway. If the baby is attempting to cough but is unable to, it may indicate a severe obstruction. If the baby has only minimal cough attempts or has completely stopped coughing, you need to help the baby open the airway rather than waiting for it to open on its own.
- Skin or lips turning blue or pale
A change in skin tone, especially around the lips or face, is a late and serious sign of choking. It indicates that the baby isn’t getting enough oxygen. This symptom requires urgent attention. Begin first aid immediately and call for emergency help if necessary.
- Difficulty breathing or noisy breathing
If your baby is struggling to breathe, gasping, or making high-pitched noises, it suggests a partial airway obstruction. Even if the baby can still draw some breath, this situation can worsen quickly, so it’s essential to stay alert and ready to act.
- Panic or flailing arms
A choking baby may look scared or begin waving their arms in panic. This physical distress is often an instinctive reaction to the sudden inability to breathe correctly. It’s crucial to stay calm, as a quick and composed response can help your baby recover more quickly.
Recognising these signs early allows you to respond immediately with the correct first aid techniques, such as back blows and chest thrusts, before professional help arrives. The faster you act, the better the chances of clearing the blockage and preventing serious complications.

Common Causes of Baby Choking
Choking can occur in various situations, and some are more common than others. Understanding the potential causes can help parents, carers, and childcare professionals reduce the risk. Below are some of the most common choking hazards for babies and young children:
| Cause |
Description |
| Choking on milk |
Newborns and infants can choke on milk, especially if they feed too quickly or lie flat while feeding. |
| Small food items |
Foods like grapes, nuts, chunks of meat, and hard candies can block the airway if not prepared correctly. |
| Toys and household objects |
Small items like coins, buttons, beads, and toy parts can easily become choking hazards for babies and toddlers. |
| Improper feeding techniques |
Overfilled bottles or fast-flow nipples cause babies to swallow too much at once, increasing choking risks. |
| Feeding in a lying-down position |
Feeding in this position increases the risk of choking as milk can flow into the wrong airway. |
| Lack of supervision |
Choking often happens when babies are left alone, even for a short time, while eating or playing. |
| Sticky or chewy foods |
Foods like peanut butter, marshmallows, and certain candies can get stuck in the airway, particularly for younger children. |
| Playing with small toys |
Babies and toddlers often put small toys or toy parts in their mouths, creating choking hazards. |
| Poorly cut food |
Large chunks of food or food that’s not appropriately cut can block a baby’s airway, leading to choking. |
| Sudden distractions |
Distractions during feeding or play can cause babies to accidentally swallow or put objects in their mouths too quickly, leading to choking. |
What to Do If Your Baby is Choking: A Step-by-Step Guide
When a baby chokes, acting quickly and calmly can save their life. The following steps are based on NHS guidelines and are designed to be clear and actionable for all carers.
1. Assess the situation:
If the baby can still cough or cry, allow him/her to continue what he/she was doing, as this helps dislodge the obstruction. If the baby cannot make any sounds (cries or coughs) or is turning blue from lack of breath, you need to act immediately
2. Call for Help:
Call 999 or 112 for emergency assistance. If you are busy helping your baby, ask someone nearby to call for you.
3. Position the Baby:
For infants under 1 year old, lay the baby face down along your forearm, supporting the head and neck. Ensure the head is lower than the chest.
4. Administer Back Blows:
Using the heel of your hand, give up to five sharp back blows between the baby’s shoulder blades. Check after each blow to see if the object has been dislodged.
5. Perform Chest Thrusts:
If the blockage remains, turn the baby face-up, keeping the head lower than the chest. Place two fingers in the centre of the chest, just below the nipple line. Give up to five sharp chest thrusts.
6. Repeat if Necessary:
Continue alternating back blows and chest thrusts until the object is expelled or emergency help arrives. If at any point the baby becomes unresponsive and is not breathing, begin infant CPR.
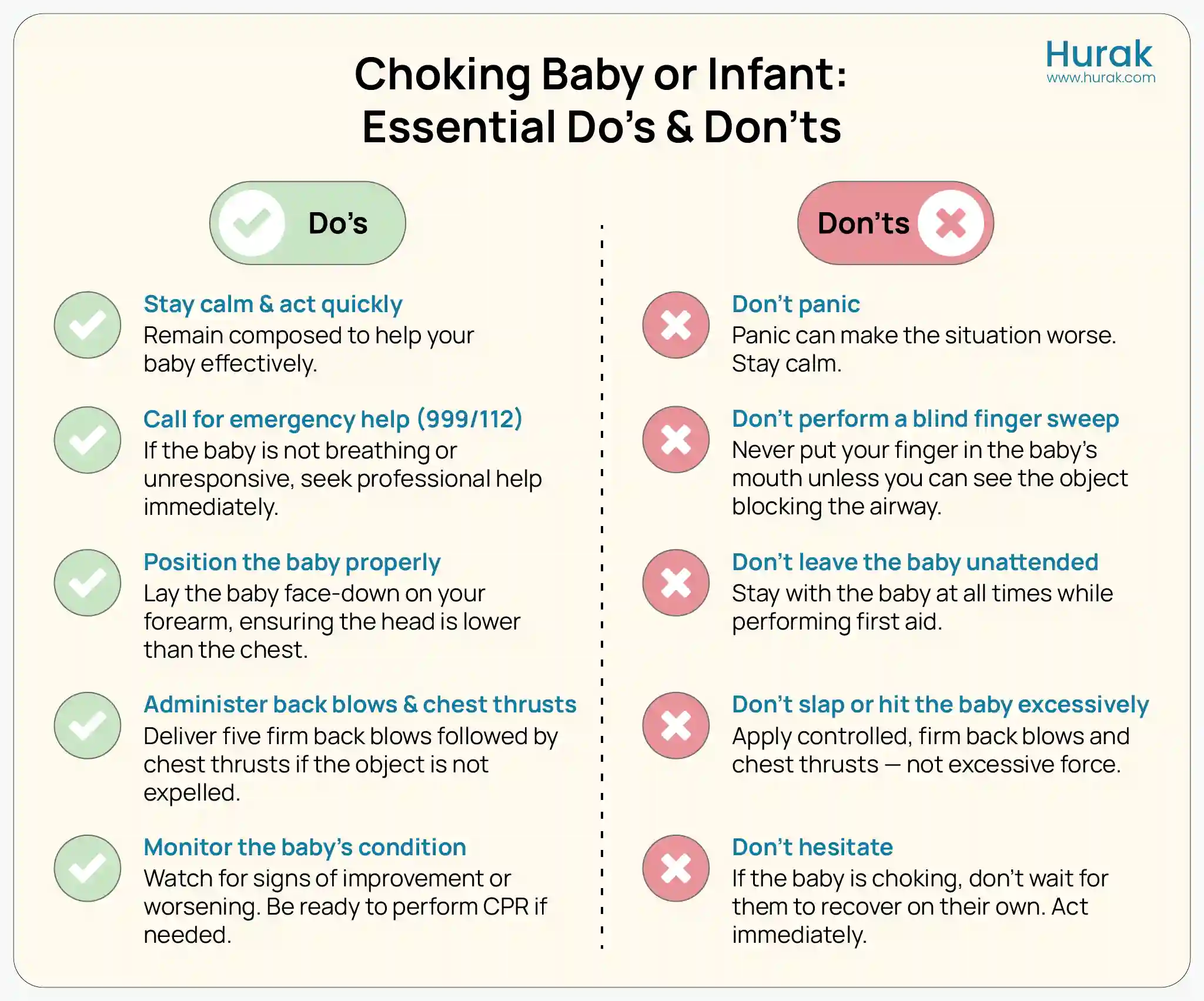
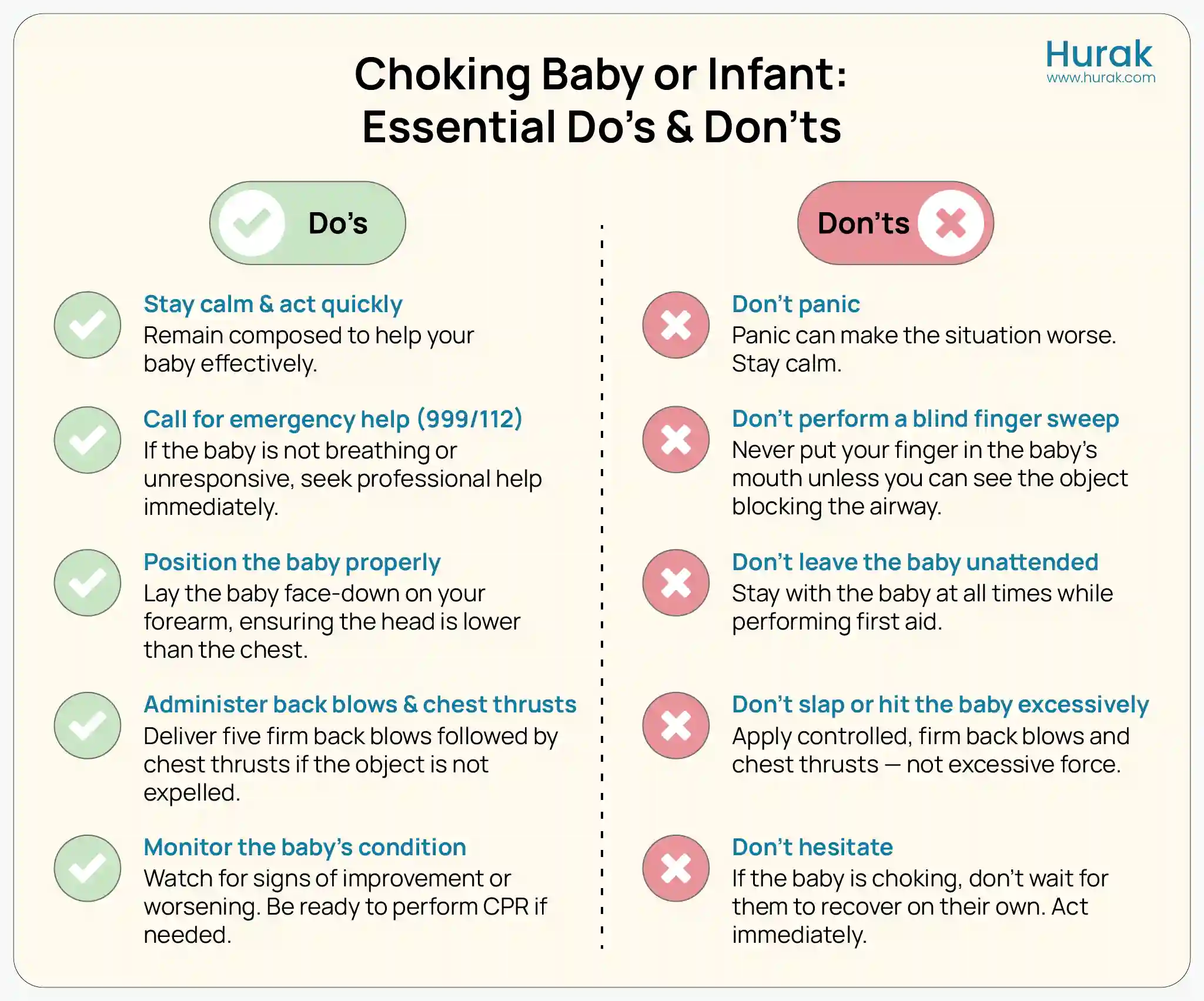
Below is a visual checklist of the essential do’s and don’ts to follow when handling a choking baby or infant:
Prevent Choking in Infants
Prevention is always better than dealing with a choking emergency. Here are simple steps to reduce the risk of your baby choking:
- Supervise feeding and play: Always supervise the baby while they eat or play. Don’t leave an infant or toddler alone and unattended with small objects or food.
- Feed in the correct position: When feeding your baby, you should hold them slightly upright. Whether the baby is bottle-fed or breastfed, you want to make sure you burp them often to prevent milk from coming back up quickly.
- Offer age-appropriate foods: Don’t give babies under 4 years anything small, complex, or round like nuts, grapes, popcorn, or hard candies. For soft foods, cut them into tiny, manageable pieces.
- Offer age-appropriate foods: Store small items such as coins, buttons, and small toy pieces on high surfaces so babies cannot reach them, and check your floors and the surfaces below them for potential choking hazards regularly.
- Stay up-to-date with first aid for baby choking: It is essential for parents, caregivers, and childcare providers to stay up to date with first-aid training pertaining to infants who are choking. Take a first-aid certification course to be confident and knowledgeable about how to respond in an emergency.
Conclusion
Choking can happen suddenly, and every second counts when a baby’s airway is blocked. Understanding the signs of choking, knowing what to do if your baby is choking, and learning the correct positioning for back blows and chest thrusts can save a life.
Parents, carers and childcare professionals choosing the best first aid training qualification play vital roles in keeping babies safe. While emergency first aid is vital, prevention is equally important; supervising feeding, offering age-appropriate foods and keeping small objects out of reach can significantly reduce risks
Frequently Asked Questions
How should you position a choking infant when you begin to treat them?
Hold the baby face down along your forearm, supporting the head and neck. Keep the head lower than the chest for a back blow. If chest thrusts are needed, turn the baby face-up while still supporting the head and neck.
How to stop a baby choking?
Back-to-back five blows and five chest thrusts for infants under 1 year. Call emergency services if the baby cannot breathe or becomes unresponsive. Avoid finger sweeps unless the object is clearly visible.
What to do if a newborn chokes on milk?
Sit the baby slightly upright during feeding and burp regularly. If choking occurs, follow the back blows and chest thrust sequence. Call emergency services if the baby cannot clear the milk and shows signs of distress
When should you seek medical help after a choking incident?
Seek medical attention even if the baby seems fine afterwards. Call emergency services immediately if the baby cannot breathe or coughs or turns blue. Newborns choking on milk or other fluids should always be assessed by a healthcare professional.
Explore Other First Aid Courses at Hurak
Looking to boost your skills? Explore our range of first aid courses to find the right one for you.
Here are some of our most popular first aid courses to help you stay prepared:
- Emergency First Aid at Work (1 Day): A one-day course covering essential life-saving skills, including CPR, choking, bleeding control, and managing emergencies. Ideal for low-risk workplaces.
- First Aid at Work (3 Days): A comprehensive three-day training that prepares you to respond to a wide range of injuries and illnesses in the workplace. Meets HSE requirements for high-risk environments.
- Paediatric First Aid (2 Days): Designed for those working with infants and children. Covers child-specific emergencies like choking, febrile seizures, allergic reactions, and more.
- Basic First Aid Course: Perfect for general awareness. It covers basic skills like dealing with minor wounds, burns, shock, and fainting and is suitable for non-workplace settings.
- Advanced First Aid Training: Intended for those needing higher-level skills. Includes oxygen administration, advanced trauma management, and secondary assessments.
- First Aid for Mental Health: Focuses on identifying, understanding, and supporting individuals with mental health conditions. Covers stress, anxiety, depression, and early intervention strategies.