Borderline Personality Disorder (BPD) affects thousands of people across the UK. Yet, it remains surrounded by stigma and confusion. Many struggle for years before receiving a diagnosis or the support they need, often misunderstood by both professionals and loved ones.
This article aims to clarify Borderline Personality Disorder (BPD) by providing a clear and compassionate overview of its symptoms, causes, and the treatment pathways available through the NHS (National Health Service) and other support networks. With the right understanding and care, recovery is not only possible, it’s within reach.

What is BPD?
Borderline Personality Disorder (BPD) is a deeply challenging mental health condition that influences how a person experiences emotions, views themselves, and connects with others. It’s often associated with overwhelming emotional shifts, unstable relationships, impulsive actions, and confusion about self-identity.
Many individuals with BPD live with an intense fear of being abandoned, frequent mood swings, and difficulty regulating emotions. These struggles can make everyday situations feel unpredictable and relationships emotionally draining.
The good news is that BPD is highly treatable. With the right therapeutic support, structure, and self-understanding, people with BPD can find balance and lead meaningful, fulfilling lives.
What Are the Signs and Symptoms of BPD?
Borderline Personality Disorder (BPD) affects how individuals experience emotions, relationships, and self-identity. While symptoms can vary from person to person, there are several common signs that mental health professionals look for when diagnosing BPD.
Below are the key symptoms associated with BPD:
|
Signs and Symptoms |
Description |
|
Intense Fear of Abandonment |
People with BPD often go to great lengths to avoid real or perceived abandonment. Even minor changes in plans or tone of voice can trigger anxiety or distress. |
|
Unstable Relationships |
Relationships tend to be intense and short-lived. Individuals may quickly shift between idealising someone and suddenly devaluing them. |
|
Distorted Self-Image |
A person with BPD may struggle with a fragile or shifting sense of identity, unsure of who they are, what they believe, or how they see themselves |
|
Impulsive Behaviours |
A person with BPD may struggle with a fragile or shifting sense of identity, unsure of who they are, what they believe, or how they see themselves |
|
Emotional Instability |
Mood swings are intense and unpredictable, shifting rapidly from joy to anger, anxiety, or despair, lasting hours to days. |
|
Chronic Feelings of Emptiness |
Many with BPD feel persistently “empty” inside and may seek stimulation or relationships to fill the void. |
|
Inappropriate or Intense Anger |
Sudden outbursts of anger, sarcasm, or aggression often occur, especially when feeling rejected or misunderstood. |
|
Stress-Related Paranoia |
Short episodes of mistrust, suspicion, or distorted thinking are triggered by emotional stress, especially in sensitive situations. |
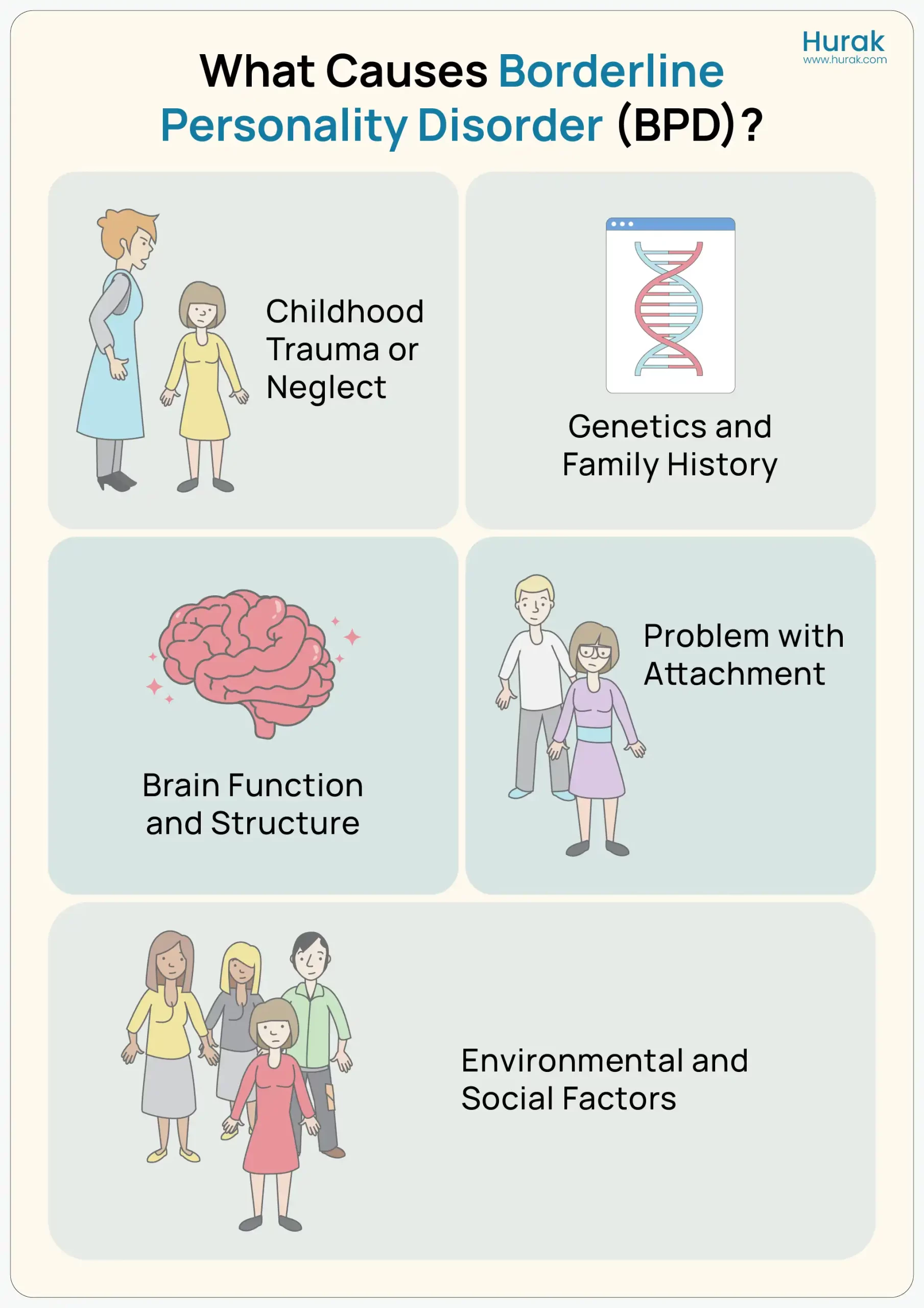
What Causes BPD?
There’s no single cause of Borderline Personality Disorder. Instead, it’s believed to develop from a combination of genetic, environmental, and social factors. Understanding the possible causes can help reduce stigma and promote a more compassionate view of the condition.
Here are some of the key contributing factors:
Childhood Trauma or Neglect
Many people with BPD report experiencing early trauma, such as abuse (emotional, physical, or sexual), neglect, abandonment, or prolonged separation from a caregiver. These early disruptions in emotional development may make it harder to form stable relationships or regulate emotions later in life.
Genetics and Family History
BPD tends to run in families. If a close family member, such as a parent or sibling, has BPD or another mental health condition, the risk may be higher. This suggests a possible genetic link, although no specific “BPD gene” has been identified.
Brain Function and Structure
Research using brain imaging suggests that people with BPD may have differences in the areas of the brain that control emotion, decision-making, and impulse regulation, particularly the amygdala, hippocampus, and prefrontal cortex. These differences might contribute to emotional sensitivity and impulsivity.
Problems with Attachment
Difficulties forming healthy emotional bonds in early childhood, especially inconsistent or invalidating caregiving, may lead to attachment issues, a key feature in the development of BPD. Individuals may struggle with trust, self-worth, and emotional safety in relationships.
Environmental and Social Factors
Stressful life events such as bullying, domestic violence, long-term instability, or growing up in a chaotic or invalidating environment can all increase the risk of developing BPD. These experiences may interfere with emotional development and coping skills.
The infographic below illustrates the key points:
Borderline Personality Disorder Treatments
Living with Borderline Personality Disorder can be difficult, but there is hope. With access to the right therapy, emotional support, and self-care tools, many people with BPD go on to live rewarding, stable lives. Treatment is focused on emotional regulation, relationship skills, and reducing distressing behaviours, and is widely available in the UK through the NHS or private mental health services.
Dialectical Behaviour Therapy (DBT)
DBT is one of the most effective and commonly recommended treatments for BPD. It focuses on four key areas:
- Emotional regulation
- Distress tolerance
- Mindfulness
- Interpersonal effectiveness
It helps people manage intense emotions and develop healthier coping skills.
Mentalisation-Based Therapy (MBT)
MBT helps individuals understand their thoughts and feelings and those of others more clearly. It’s especially helpful for improving relationships and emotional stability.
Cognitive Behavioural Therapy (CBT)
CBT is not a primary treatment for BPD, but may help with related issues like anxiety, depression, or impulsive behaviours.
Schema Therapy
This therapy focuses on identifying and changing deep-rooted patterns and beliefs formed in childhood that may be contributing to BPD symptoms.
Important Note:
There is no specific medication approved for treating BPD itself. However, doctors may prescribe medication to manage associated symptoms, such as:
- Mood swings
- Anxiety
- Depression
- Sleep disturbances
Frequently Asked Questions (FAQs):
What is Borderline Personality Disorder (BPD)?
BPD is a mental health condition that affects how a person manages emotions, relates to others, and sees themselves. It often involves emotional instability, impulsive behaviour, and difficulties in relationships.
Is BPD treatable?
Yes, BPD is treatable. With the right support — such as talking therapies like DBT or MBT, and ongoing care through the NHS or private services — many people see real improvements in how they cope and connect with others.
What causes BPD?
There isn’t one single cause. BPD is usually linked to a mix of factors, including childhood trauma, genetics, brain chemistry, and early attachment issues. Everyone’s experience is different.
How is BPD diagnosed in the UK?
A diagnosis is usually made by a GP or mental health professional based on your symptoms and history. You may be referred to a community mental health team (CMHT) for a full assessment.
Can people with BPD live normal lives?
Absolutely. With the right treatment, self-care, and support, many people with BPD build strong relationships, manage their emotions effectively, and live fulfilling, stable lives
Explore more about our courses:
Emergency First Aid at Work is described as a short, practical training course designed to prepare individuals to respond to medical emergencies in low-risk workplace settings.
First Aid at Work is a comprehensive, Ofqual-regulated Level 3 qualification delivered over three days in a classroom setting. It is ideal for first aiders working in high-risk or diverse environments such as construction sites, manufacturing units, or warehouses.
Paediatric First Aid is a two-day, Ofqual-regulated classroom-based training that specifically focuses on first aid for infants (0–1 year) and children up to puberty. It’s ideal for anyone working with or caring for young children.
Basic First Aid Course is a compact, self-paced program ideal for individuals seeking an introduction to first aid or a quick annual refresh.
Advanced First Aid Course is a fully online, self-paced Level 3 training designed for individuals seeking more comprehensive knowledge beyond basic first aid.