Does the sight of blood make you feel uneasy, anxious, stressed, and a continuous urge to look away? It might be far from just a normal anxiety. Many People experience this fear, for some people, even a quick glimpse of blood can bring on intense anxiety, dizziness, or even fainting. It can feel frightening and hard to explain, especially when others don’t have any idea what you are going through.
If you or someone close to you struggles with this, take a breath. You’re in the right place. This article is here to guide you gently through what haemophobia really is, why it happens, and most importantly, the practical and proven ways you can learn to cope with this phobia and regain a sense of control, at your own pace.
What Is Haemophobia?
The word Haemophobia is derived from the Greek words “haema”, meaning blood, and “phobos”, meaning fear. It is categorised in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) as a specific phobia. Haemophobia is also known as blood phobia, is an intense and overwhelming fear of blood. For many other people who are suffering from haemophobia, even a minimal amount of blood, such as a paper cut, can trigger their anxiety and can cause dizziness or even fainting on the spot. Although it may seem unusual, haemophobia is more common than many people can even realise.
Unlike other phobias, which trigger a surge of adrenaline, Haemophobia uniquely often leads to a biphasic response, which is a two-stage reaction or response by a person suffering from haemophobia. This means the body reacts in two distinct stages, and this is what makes the fear of blood more challenging to deal with. The two distinct stages are:
- Initial surge: When a person sees blood, the body briefly goes into alarm mode, with the heart rate increasing, blood pressure rising slightly, and feelings of fear or panic starting to appear.
- Sudden drop: It is also known as vasovagal syncope. In this situation, the heart rate and blood pressure drop quickly, reducing the blood flow to the brain. This can lead to dizziness, weakness, nausea, and in many cases, even fainting can occur. This second stage is the key feature that sets haemophobia apart from other phobias and makes it particularly distressing.
Causes of Haemophobia
Understanding what causes haemophobia is an important step towards managing it. Haemophobia does not usually develop from a single cause. It usually stems from a mix of biological factors, past experiences, and learned behaviours. The table below highlights the most common contributors to this fear.
| Cause Category |
Explanation |
Examples / Key Points |
| Genetic & Biological Factors |
Some individuals may naturally have a stronger anxiety response or a hereditary tendency towards fainting. |
• Genetic predisposition to anxiety disorders
• Inherited vasovagal reflex causing fainting at the sight of blood |
| Traumatic or Negative Experiences |
Past distressing events or even exposure to blood-related incidents can trigger long-term fear responses in an individual. |
• Witnessing accidents involving blood.
• Painful or frightening medical procedures.
• Seeing others panic or faint around blood. |
| Learned Behaviour |
Fear is developed by observing others or absorbing negative stories or experiencing blood-related reactions. |
• Family members showing fear of blood
• Hearing disturbing stories about injuries or surgeries
• Cultural beliefs or social influences that heighten the fear |
| Evolutionary Perspective |
Some theories suggest the fear and fainting response evolved as a protective mechanism during injuries. |
• Fainting reduces blood pressure to minimise blood loss.
• Strong vasovagal response in certain individuals |
Recognising the Symptoms of Haemophobia
Symptoms of haemophobia can appear when someone sees, anticipates, or even thinks about the blood. These reactions may be psychological (that is, emotional and behavioural) or physical in the body, and together they help identify the presence of this phobia.
Psychological Symptoms
These symptoms relate to a person’s emotional responses, thoughts, and behaviour in blood-related situations, such as witnessing an accident. Where that person can go through several emotional changes, such as:
- Intense Anxiety – A sudden rush of fear or panic at the sight or thought of blood.
- Strong Sense of Dread – Feeling like something bad or dangerous is about to happen.
- Avoidance Behaviour – Actively avoiding hospitals, blood tests, first-aid situations, or conversations involving blood.
- Irritability or Tension – Becoming unusually restless, agitated, or uncomfortable in blood-related contexts.
Physical Symptoms
The physical symptoms involve the body’s natural reaction to fear and, in some people, the characteristic “biphasic” pattern where blood pressure drops suddenly and can lead to:
- Dizziness or Light-headedness – Feeling faint or unsteady.
- Nausea – Stomach discomfort, sometimes leading to vomiting.
- Sweating and Pallor – Cold sweat with noticeably pale skin.
- Sudden Weakness – Limbs feeling heavy or weak.
Impact of Haemophobia
Haemophobia may appear to be a minor fear from the outside, but it can have a real impact on many areas of your life. Understanding how it affects your day-to-day life helps explain why proper support and treatment really matter. Some key impacts you might experience in your day-to-day life, which include:
- Avoiding medical care: If you are delaying or completely avoiding blood tests, vaccinations, or routine health check-ups because of your blood fear.
- Fainting and weakness: If you are experiencing sudden dizziness or fainting episodes, this can increase the risk of falls or injuries.
- Daily anxiety: Constant worry about encountering blood or blood-related situations can raise stress levels and affect your emotional well-being.
- Avoidance behaviours: If you steer clear of hospitals, first-aid situations, medical discussions, or even television shows that show blood.
- Lifestyle limitations: Fear of getting injured and seeing blood may stop you from taking part in sports, exercise, or other physical activities in your day-to-day life.
When to Seek Professional Help
It is very important to reach out to any professional support when haemophobia begins to affect your daily functioning or feels too overwhelming to manage. A mental health professional can help you by understanding your symptoms and guiding you towards effective treatment options, which can eventually help you manage your phobia. Here are some important flags that you must keep your eyes on, and seek professional help as soon as possible are:
- When fear interferes with medical care and stops you from getting essential treatment.
- You may faint, even at the sight or thought of blood.
- Anxiety becomes difficult to manage alone.
- The phobia starts impacting your daily life or relationships.
Taking early actions can lead to better outcomes, so addressing the symptoms at an early stage that you notice can help prevent them from becoming severe over time. Early support or treatment makes it easier for you to develop healthy coping strategies by reducing avoidance behaviours and managing anxiety more effectively.
Diagnosis of Haemophobia
A diagnosis of haemophobia is usually made by a qualified mental health professional who assesses how severe the fear is and how it affects your daily life. This assessment may be carried out by a psychologist, psychiatrist, or a GP with experience in anxiety disorders.
The diagnosis is typically based on several factors. These include a review of your medical history to identify any past experiences or triggers you were facing, a detailed description of your symptoms and how they may appear in blood-related situations, and an evaluation of how long the fear has been present in you and whether it interferes with your everyday activities. Health professionals will also rule out medical conditions, such as heart or blood pressure issues, that could explain symptoms like dizziness or fainting.
To confirm the diagnosis, professionals often refer to the DSM-5 criteria for specific phobias. This helps to ensure that the symptoms are linked to an anxiety-based phobia rather than a physical health condition.
Treatment and Overcoming the Fear
Fortunately, haemophobia is highly treatable. When it’s addressed early, treatment tends to work even better. The most effective approaches focus on both sides of the fear, that i,s psychological anxiety around blood and the physical fainting response. It can help people feel more in control and confident over time.
Applied Tension Technique (ATT)
This is a specific behavioural technique developed to check your blood pressure drop, which can lead to fainting. It involves tensing the major muscle groups (arms, legs, torso) for 10-15 seconds, then relaxing for 20-30 seconds, and repeating the same until the feeling of warmth or faintness subsides. ATT works by temporarily increasing blood pressure, helping to maintain blood flow to the brain and prevent syncope.
Cognitive Behavioural Therapy (CBT)
CBT helps you to identify and challenge the negative thought patterns and irrational beliefs that are associated with blood. A therapist can assist in restructuring these thoughts, which will help you to reduce anxiety.
Exposure Therapy
This is a core component of treating specific phobias. Under the guidance of a therapist, you will gradually and safely be exposed to blood-related triggers, starting with less frightening stimuli (e.g., pictures of blood) and progressing to more challenging situations (e.g., watching a medical procedure).
Relaxation Techniques
Practices such as deep diaphragmatic breathing and progressive muscle relaxation can help manage the initial surge of anxiety before the blood pressure drop occurs.
Self-Help Tips for Managing Haemophobia
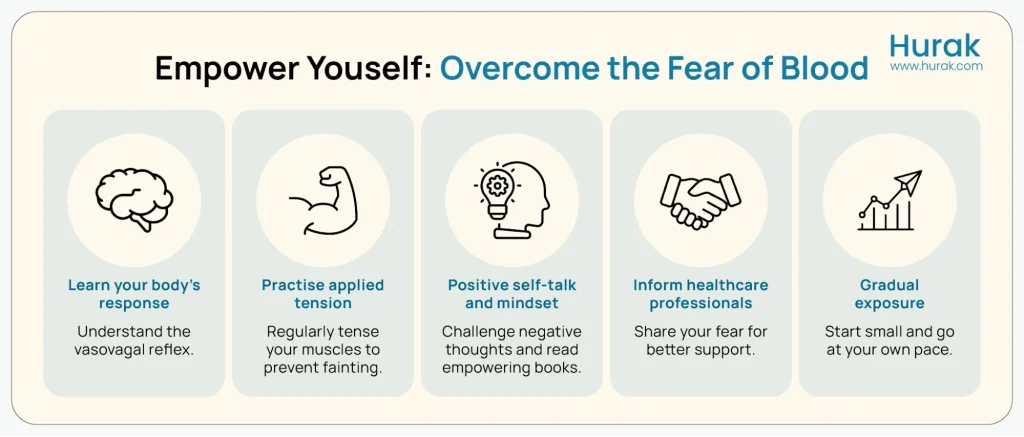
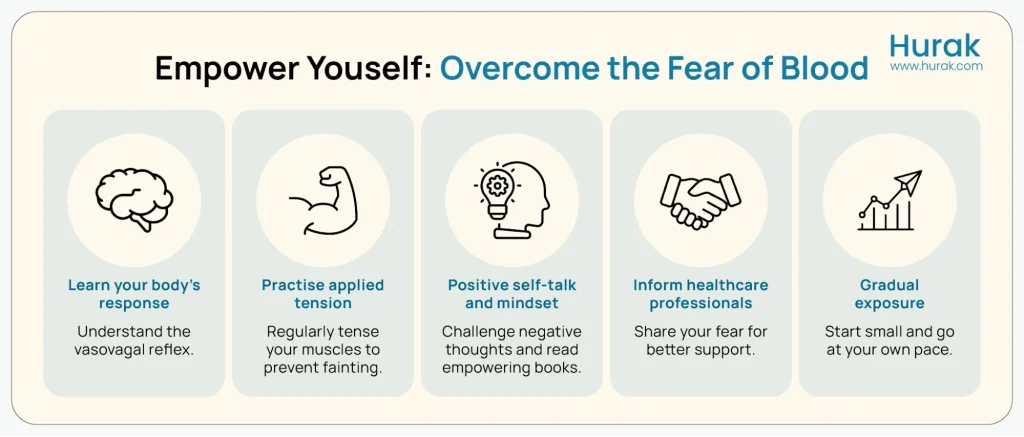
While professional support can be helpful, there are also simple techniques you can practise on your own to gradually reduce fear and build confidence. These strategies can make everyday situations more manageable and support your progress over time. These are some useful self-help tips for you to manage haemophobia:
- Learn about the body’s natural response to blood
- Practise applied tension regularly
- Use positive self-talk,and read books which can help you feel free mentally.
- Share your fear with healthcare professionals so they can support you
Conclusion
Haemophobia is challenging due to its potential for fainting, but it is not a life sentence. It is a highly studied and well-understood condition, and effective, science-backed treatments are fortunately available for anyone who is suffering from haemophobia.
Haemophobia can feel overwhelming, but it is highly treatable. With the right support, whether through CBT, exposure therapy, applied tension, or simple self-help practices, people can significantly reduce their fear and regain confidence in everyday situations. Understanding your fear is the first step towards overcoming it, and many individuals go on to manage or completely overcome haemophobia with time, patience, and guidance.
Frequently Asked Question(FAQs)
Is Haemophobia truly curable, or is it just manageable?
It is one of the most successfully treated phobias. Many people experience a significant reduction or elimination of the response, allowing them to lead unrestricted lives.
Is the fear of blood a common phobia?
Yes, the fear of blood (B-I-I phobia) is considered one of the most common specific phobias, affecting a notable portion of the population.
Why does this phobia specifically cause me to faint, unlike other fears?
It triggers the unique vasovagal response, causing a sudden, dramatic drop in heart rate and blood pressure. This reduces blood flow to the brain, leading to dizziness and fainting (syncope).
Can I use the Applied Tension Technique (ATT) by myself, or do I need a therapist?
While you can practice it alone, professional guidance is highly recommended to ensure you perform it correctly and safely, especially when first learning the technique.
Can Haemophobia affect my ability to have children or receive essential surgery?
Yes. If severe and untreated, it can complicate important life events like necessary surgeries, childbirth, and fertility treatments, making treatment essential for accessing care.
Does my fear of blood mean I am generally an anxious person?
Not necessarily. Haemophobia is a specific phobia. You can be calm in most situations, as the intense anxiety is usually limited to triggers involving blood, injury, or injections.