Anaphylaxis represents a frequent medical emergency, including a life-threatening acute hypersensitivity response. This condition is marked by a widespread allergic reaction affecting multiple bodily systems. If left untreated, anaphylaxis can quickly lead to respiratory failure and even death.
What is Anaphylaxis
Anaphylaxis is a severe allergic reaction that leads to a life-threatening condition. It causes systemic shock, leading to impaired respiratory function.
Symptoms of an anaphylactic allergic reaction may include angioedema (swelling) affecting the face, neck, tongue, or lips.
Respiratory distress can occur, potentially leading to shock, including hypotension and altered consciousness.
What are the Causes of Anaphylaxis
Anaphylaxis is triggered by various allergens, which are substances that provoke an allergic reaction. Common triggers include:
- Food: Peanuts, tree nuts (such as almonds and cashews), shellfish, milk, eggs, soy, and wheat.
- Insect Venom: Bee stings, wasp stings, and other insect bites.
- Medications: Antibiotics (like penicillin), nonsteroidal anti-inflammatory drugs (NSAIDs), and certain vaccines.
- Other Substances: Latex, chemicals, and even exercise-induced factors in some individuals.

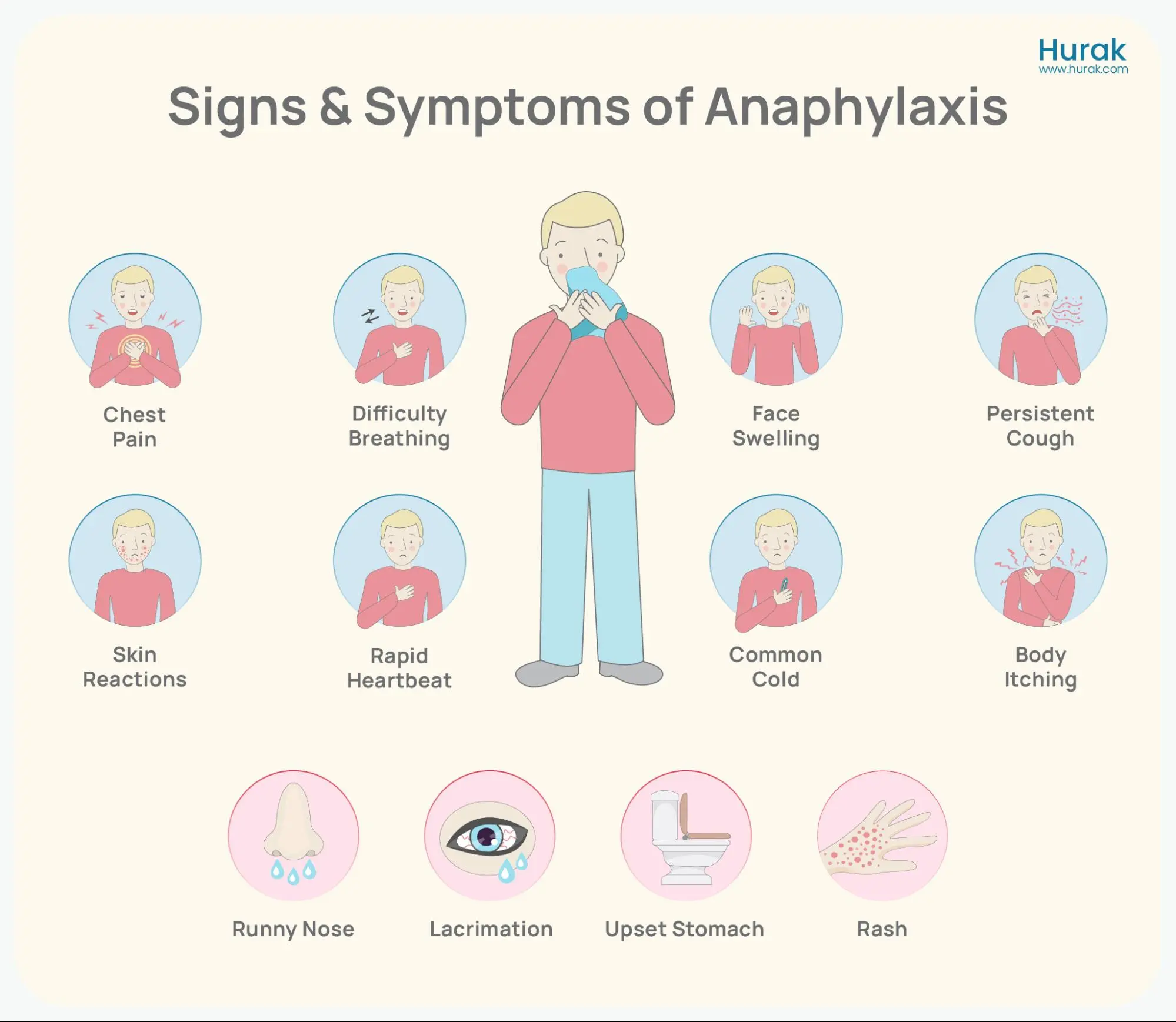
What are the Signs and Symptoms of Anaphylaxis
The signs and symptoms of anaphylaxis can develop rapidly and affect multiple organ systems:
- Respiratory System: Difficulty breathing, wheezing, throat tightness, and coughing.
- Cardiovascular System: Drop in blood pressure (hypotension), weak or rapid pulse.
- Skin: Itching, hives symptoms (urticaria), redness, and swelling (angioedema) of the face, lips, tongue, or throat.
- Gastrointestinal System: Nausea, vomiting, abdominal pain, and diarrhoea.
- Neurological System: Dizziness, confusion, and loss of consciousness.
What are the Stages of an Allergic Reaction?
Allergic reactions generally involve several stages, varying in severity and duration depending on the individual and the allergen involved. Here are the typical stages:
- Exposure: This is the initial stage where the person comes into contact with the allergen, whether through ingestion, inhalation, skin contact, or injection (as with insect stings).
- Sensitisation: In this stage, the immune system recognises the allergen as a threat and starts producing specific antibodies against it (IgE). This sensitisation process may occur over time and can involve repeated exposures to the allergen.
- Activation: Upon exposure to the allergen, the antibodies trigger the release of chemicals such as histamine from mast cells and basophils in the body. This release leads to the onset of allergic symptoms.
- Occurrence of Symptoms: This stage involves an allergic reaction, which can vary widely depending on the allergen and the individual’s immune response.
Symptoms can affect various systems, including:
- Skin (itching, hives)
- Respiratory system (wheezing, difficulty breathing)
- Gastrointestinal system (nausea, vomiting)
- Cardiovascular system (rapid heartbeat, drop in blood pressure).
5. Resolution: The symptoms typically disappear after removing or neutralising the allergen (e.g., by medications like antihistamines or epinephrine).
The resolution stage may vary in duration, depending on the reaction’s severity and the treatment’s effectiveness.
Get Trained in All First-Aid Skills
First Aid Courses
Book NowRated Excellent
on major review sites

How is Anaphylaxis Prevented
Prevention of Anaphylaxis is important for immuno-compromised people, who are vulnerable to allergens. Preventing anaphylaxis involves:
- Medical Alert Identification: Wear medical alert jewellery (e.g., bracelets) indicating allergies and carry an epinephrine auto-injector.
- Education: Educate oneself and others about triggers, symptoms, and emergency response protocols.
- Allergy Testing: Undergo allergy testing to identify specific triggers and develop a management plan with healthcare providers.
- Food Allergy Management: Properly managing allergens during food processing and packaging is crucial to prevent cross-contact contamination. Key methods for allergen control include:
- Clear Allergen Labelling
- Proper Refrigeration
- Staff and Equipment Hygiene
- Colour-Coded Utensils
- Implementing the HACCP System: Process and Principles
What is the Treatment of an Anaphylactic Allergic Reaction
Immediate treatment of anaphylaxis involves administering epinephrine (adrenaline) via an auto-injector device (such as an EpiPen) to counteract the allergic response. Additional measures may include:
- Monitoring: Continuous monitoring of vital signs (blood pressure, pulse, and oxygen saturation).
- Supportive Care: Medicinal treatment includes oxygen therapy, intravenous fluids to maintain blood pressure, and medications like antihistamines and corticosteroids to reduce inflammation.
- Emergency Medical Attention: Prompt transfer to a hospital emergency room for further evaluation and management.
Ready to Learn More?
Knowing how to manage anaphylaxis is important in emergencies, but there's more to first aid. Our First Aid courses offer complete training to help you handle critical situations. Whether you want to improve your skills or workplace safety, these courses help build confidence and expertise. View our Emergency First Aid at Work (EFAW) and Level 3 First Aid at Work courses. These courses meet the UK legal requirements and help you keep people safe.
What are the Types of Anaphylactic Reactions
Anaphylaxis can be classified into different types based on triggers and clinical presentation:
- Food-Induced Anaphylaxis: Triggered by ingestion of allergenic foods.
- Insect Sting Anaphylaxis: Caused by venom from insect stings or bites.
- Drug-Induced Anaphylaxis: Reaction to medications or vaccines.
- Exercise-Induced Anaphylaxis: Triggered by physical exertion in conjunction with specific factors.
- Idiopathic Anaphylaxis: Cases where the trigger is unknown.
Conclusion
Anaphylaxis is a serious allergic reaction that must be immediately identified and treated to prevent life-threatening complications. Understanding the causes, signs, treatment options, triggers, types, and prevention strategies empowers individuals to effectively manage and reduce the risks associated with anaphylaxis. For those with known allergies, proactive measures are essential to ensuring safety outcomes in an anaphylactic emergency.




